Science has shown that β-carotene, has benefits beyond being a source of Vitamin A, but the benefits have been difficult to reproduce.
Avivagen is changing this.
Did you know?
Did you know antibiotic resistance in humans is considered to be this century’s single greatest global health threat? The cause is the widespread use of antibiotics in animal feeds to produce meat consumed by humans, as well as over-prescription by physicians for therapeutic treatment of human infections. Avivagen has an alternative.
The Evidence: Trials
OxC-beta Livestock has undergone extensive field trial and customer evaluations in dairy cattle, pigs and broiler poultry at research centres and customer facilities around the world. Results from these trials demonstrate that OxC-beta Livestock supports immune function and overall animal health, leading to significant benefits in productivity. The bottom line is healthier animals perform better.
40+ clinical and field trials




β-Carotene and the more than 600 other members of the carotenoid family are characterized by an extended system of conjugated carbon-carbon double bonds that provide intense colour and make the compounds highly susceptible to reaction with oxygen in air.
The purported benefits of non-vitamin A effects of β-carotene include improved immune function. A summary of literature results for supplementation with β-carotene has been provided in a European Food Safety Authority panel report on the safety and efficacy of β-carotene as a feed additive [2]:
“The positive effects in cows or pigs reported in the literature include decreased service per conception, increased number of viable embryos/reduced embryonic mortality, improved embryo quality, improved immunity with reduced incidence of retained placenta and metritis, increased pregnancy rate, increased percentage of milk fat (with unaffected milk yield), improved protection of the mammary gland against infection as a result of increased intracellular killing of microbes by phagocytes, and higher plasma progesterone and oestradiol levels in the cat…”. “Chew and co-workers reported that beta-carotene improves the immune status and decreases the incidence of reproductive disorders in peripartum cows by increasing lymphocyte and phagocyte function…”.
However, the EFSA panel further states:
“The data on the effects of supplemented β-carotene on immunity and reproduction remain inconsistent and no conclusions can be drawn”. This comment underscores the lack of reproducibility of data when β-carotene itself is used as the supplement. Also, the possible inadvertent involvement of vitamin A is cited as a confounding factor.
The β-carotene copolymer compound, as well as other carotenoid copolymer compounds, and their apocarotenoid breakdown products are ubiquitous, being formed naturally in variable and often significant quantities in carotenoid-containing plant materials, especially during processing, such as dehydration, and during storage. This is simply the result of exposure to air. Naturally occurring examples relevant to livestock feeds include alfalfa, grass and seaweed products, and in human nutrition, carrot and tomato powders [4].
Illustration of the effect of dehydration and storage on β-carotene oxidation in carrots. The formation in dehydrated, powdered carrot of geronic acid, a marker of β-carotene oxidation and the associated copolymer products, can be seen to be closely linked to the concomitant loss of β-carotene.
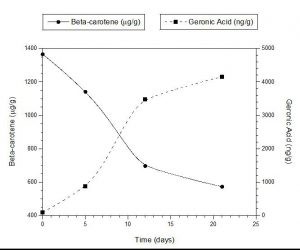
Corroboration of the natural occurrence of OxBC has been provided independently by Schaub, Beyer and co- workers [5]. In accounting for the loss of β-carotene in an extensive variety of β-carotene plant crop foods during storage, this group reported that spontaneous oxidation of β-carotene leads to the concurrent formation of β-carotene copolymer compounds as the major product.
Avivagen manufactures OxBC (Oxidized β- Carotene) by allowing pure β-carotene dissolved in a solvent to react fully with oxygen from air. OxBC is composed entirely of oxidation products comprised of β-carotene-oxygen copolymers and their apocarotenoid breakdown products. No β-carotene remains. No vitamin A is formed and there is no vitamin A activity. The immune-supporting activity of OxBC demonstrates that β-carotene’s non-vitamin A effects arise directly from β-carotene’s oxidation products [3].
The benefits are clear and consistent when OxBC is provided orally to livestock and dogs. There is immune function support as previously associated with β-carotene. This discovery explains why β-carotene is unable to fulfil this function itself unless it first has undergone spontaneous oxidation to form OxBC. In poultry and swine, benefits are obtained at just low parts-per-million levels of OxBC in finished feed, well within the limits of levels of β-carotene were it available from plant sources, and quite apart from and complementary to the effects of supplemental vitamin A.
Avivagen is now providing this product in three ways—a supplement called OxC-beta™ Livestock for livestock feeds, into Vivamune™, Oximunol™ and Dr Tobias All-in-One Dog Chews supplements for pets, and in the Beta Blend product for humans.
A breakthrough product for livestock feeds
In animal nutrition, β-carotene has been primarily regarded as a source of vitamin A. Originally, vitamin A was provided by adding certain β-carotene-rich plant materials or forages to livestock feeds. The challenge is there is a significant loss of β-carotene and vitamin A during processing and storing. As a result, natural sources of β-carotene have been replaced in modern livestock feeds with supplements that provide consistent levels of synthetic vitamin A instead, along with other vitamins, micronutrients and minerals. This means that most modern livestock feeds lack or are deficient in β-carotene and, therefore, β-carotene-oxygen copolymer compounds, and possibly other phytonutrients. For livestock, this dietary difference can contribute to poorer health.
Health benefits for livestock
Feeding trials in multiple animal species show the benefits of providing supplemental OxBC in the form of OxC-beta™ Livestock, over and above supplemental vitamin A. Trial results, together with supporting in vitro studies, clearly point to the β-carotene oxidation products in OxBC being the actual source of the benefits seen in livestock health. When OxC-beta Livestock is added to livestock feed, the mixture of the small molecule and copolymer compounds in OxBC increases feed consumption because of its flavour and supports immune function for better overall health.
Avivagen’s scientists have demonstrated the health benefits of OxC-beta™ Livestock in trials with thousands of animals in different countries and under a variety of conditions. These outcomes are consistent with this supplement containing the oxidized form of β-carotene contributing to a better-balanced feed ration by compensating for the lack or deficiency of what is a previously unrecognized dietary forage component.
A breakthrough product for pets
Vivamune™ chews and, more recently, Dr Tobias All-in-One Dog Chews have been available for dogs for more than eleven years. Almost 1.5 million administrations clearly show the benefits of a healthier skin and coat, better joint function, increased mobility and normal intestinal function.
Oxidation of β-carotene is a unifying concept that explains both the micronutrient’s vitamin A and non-vitamin A activities.
A breakthrough product for humans
On February 21, 2021, a new Avivagen product for humans hit the market—it’s called Beta Blend and it is a Dr. Tobias exclusive formula for providing advanced immune support. This new product is just the beginning because Avivagen is continuing to work on new products that will help people live their best life.
Research articles on OxBC have been published in several highly-respected scientific journals. See for yourself below.
- Burton, G. W.; Daroszewski, J.; Nickerson, J. G.; Johnston, J. B.; Mogg, T. J.; Nikiforov, G. B. ß-Carotene autoxidation: oxygen copolymerization, non-vitamin A products and immunological activity. J. Chem. 2014, 92, 305-316. DOI: 10.1139/cjc-2013-0494 (Open Access).
- EFSA Scientific Opinion on the safety and efficacy of beta‐carotene as a feed additive for all animal species and categories. EFSA Journal 2012, 10, 2737 (Open Access).
- Johnston, J. B.; Nickerson, J. G.; Daroszewski, J.; Mogg, T. J.; Burton, G. W. Biologically active polymers from spontaneous carotenoid oxidation. A new frontier in carotenoid activity. PLoS ONE 2014, 9, e111346 (Open Access).
- Burton, G. W.; Daroszewski, J.; Mogg, T. J.; Nikiforov, G. B.; Nickerson, J. G. Discovery and Characterization of Carotenoid-Oxygen Copolymers in Fruits and Vegetables with Potential Health Benefits. J Agric Food Chem 2016, 64, 3767-3777 (Open Access).
- Schaub, P.; Wust, F.; Koschmieder, J.; Yu, Q.; Virk, P.; Tohme, J.; Beyer, P. Nonenzymatic beta-Carotene Degradation in Provitamin A-Biofortified Crop Plants. J Agric Food Chem 2017, 65, 6588-6598 (an abstract of the article is available at: https://pubs.acs.org/doi/abs/10.1021/acs.jafc.7b01693).

